Researchers unveil promising hepatitis C vaccine design
The new approach to vaccine design may also prove useful in developing a potential vaccine against the SARS-CoV-2 virus, which causes COVID-19.
April 15, 2020
LA JOLLA, CA—A new design for a vaccine against hepatitis C virus (HCV) has shown promise in early tests, according to a study from scientists at Scripps Research.
The scientists, who present their results on April 15 in Science Advances, designed an immune-stimulating particle that resembles a whole virus and is studded with modified versions of an HCV envelope protein. Mice inoculated with these virus-mimicking particles showed a stronger antibody response than when inoculated with HCV proteins on their own. The antibody response was able to block the infectivity of several other HCV strains.
“This is a proof of concept study that we hope will soon be followed by further updates and tests to bring us closer to possible clinical trials,” says study senior author Jiang Zhu, PhD, an associate professor in the Department of Integrative Structural and Computational Biology at Scripps Research.
The study was a collaboration among three Scripps Research labs: Zhu’s; the lab of Mansun Law, PhD, associate professor in the Department of Immunology and Microbiology; and the lab of Ian Wilson, DPhil, Hansen Professor of Structural Biology and Chair of the Department of Integrative Structural and Computational Biology.
Confronting an ongoing global health challenge
HCV is thought to have emerged at least hundreds of years ago as a human pathogen after “jumping” from another mammal—possibly chimpanzees, which also can be infected by the virus. HCV infects the liver and is transmitted mostly via blood exchange; about 80 percent of infections become chronic and typically end in liver cancer or liver failure. Because the infections are often “silent,” an estimated one-half of people with the disease may not know they’re infected, according to the Centers for Disease Control and Prevention.
Globalization and the emergence of practices such as blood transfusions and needle-sharing by drug users have made HCV a significant public health threat. Researchers estimate that roughly 150 million people worldwide have the infection, with large concentrations in Africa and Asia, and that it accounts for at least several hundred thousand liver-disease-related deaths annually.
Treatments for HCV have been developed. But current options are expensive, and typically aren’t used until late in the course of infection when severe liver damage has already occurred. HCV also has the potential to evolve to become resistant to drug treatments. Vaccines have been developed against HCV, but so far none has emerged successfully from clinical trials.
HCV is, somewhat like HIV and influenza viruses, a wily pathogen that evades the immune response in part by mutating rapidly. Still, about 20 percent of people who are infected manage to clear the infection on their own, which suggests that the human immune system has some ability to fight off HCV—an ability that a vaccine might be able to boost greatly.
Crafty vaccine design for a crafty pathogen
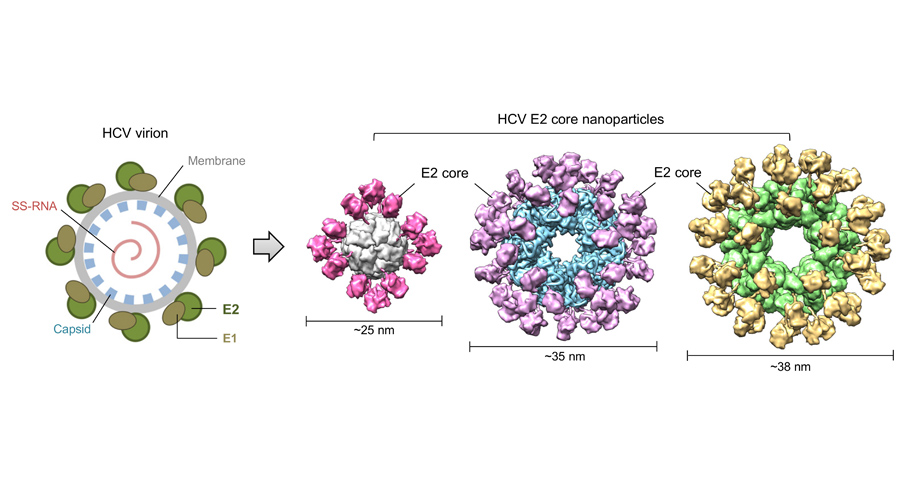
The vaccine design from Zhu and his team centers on HCV’s E2 protein. E2, in partnership with a smaller protein called E1, forms spike-like structures that stud the surface of each virus particle. E2 is the subunit of these spikes that binds to receptors on liver cells, and is the HCV protein most targeted by the immune response.
The Scripps Research team used a modified version of E2 that stabilizes its structure and omits the highly variable outer portions, leaving just the “core” portions that tend not to vary much from strain to strain because they’re needed for the virus’s efficient entry into cells.
“The idea is to remove all the distracting parts of E2 and display to the immune system only those essential structural elements where antibodies can attach to neutralize different strains,” Zhu says.
The team developed a method to mount dozens of copies of the engineered E2 proteins onto a self-assembling protein “nanoparticle” so that each of these completed creations would feel, to the immune system, more like a real virus particle.
Injected into mice, the E2-covered nanoparticles elicited stronger antibody responses than E2 proteins alone. Antibodies harvested from the mice neutralized, in lab-dish tests, HCV from two widely different groupings, or genotypes, of the virus.
The next step, Zhu says, is to create a “polyvalent” vaccine design that can confer protection against essentially all the different forms of HCV. It will use nanoparticles with E2 cores that are representative of the six major HCV genotypes. A prototype could be ready for testing in primates or even humans in a year or so, he adds.
Zhu and his team in 2018 accomplished a similar nanoparticle-based design for a vaccine against HIV. The researchers are following the same approach to develop vaccines against SARS-CoV-2, which causes COVID-19, and Ebolavirus, which causes viral hemorrhagic fever.
“This approach provides us with basic vaccine templates that we can relatively rapidly turn into prototype vaccines for testing,” Zhu says.
“Proof-of-concept for rational design of hepatitis C virus E2 core nanoparticle vaccines” was written by co-first authors Linling He and Netanel Tzarum; Xiaohe Lin, Benjamin Shapero, Cindy Sou, Colin Mann, Armando Stano, Lei Zhang, Kenna Nagy, Erick Giang, Mansun Law, Ian Wilson, and Jiang Zhu, all of Scripps Research.
Funding was provided by the National Institutes of Health (P01 AI124337, AI129698, AI140844, AI123861, AI079031, AI123365 and AI106005) and by Ufovax LLC, a spin-off vaccine company of Scripps Research, who holds exclusive rights to develop and commercialize the Scripps Research nanoparticle vaccine technology (1c-SApNP) for certain disease targets.
For more information, contact press@scripps.edu

