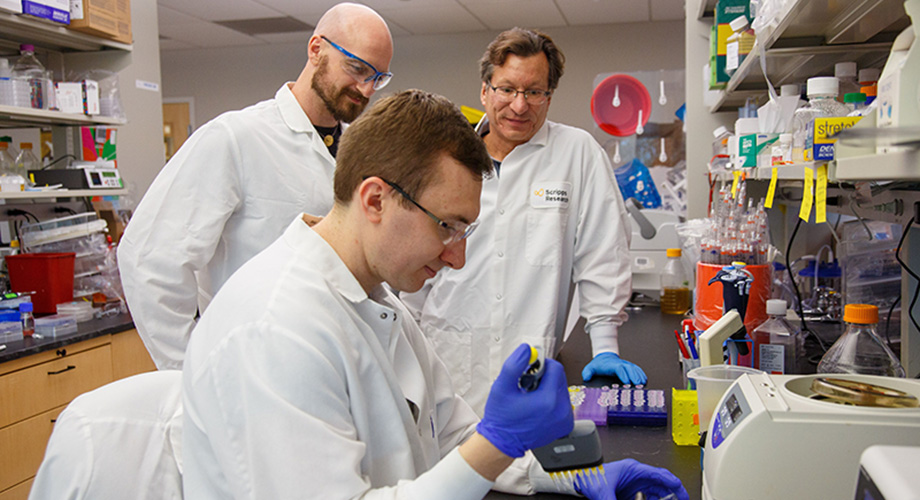
The Farzan lab’s nontraditional HIV vaccine has achieved a key milestone, defeating the “death star” strain. Co-first authors Mathew Gardner, PhD, and Christoph H. Fellinger, PhD, worked closely with mentor Michael Farzan, PhD, co-chairman of the Scripps Research Department of Immunology and Microbiology.
Viral HIV vaccine gives durable protection against tough strains
July 24, 2019
JUPITER, FL - Among HIV researchers, one seemingly indestructible HIV-like strain has earned the nickname “death star.” That’s due to the strain’s reputation for killing off hopes for potential vaccines and immunotherapies that could prevent the disease.
A team at the Scripps Research Florida campus reports successfully beating that challenge. In a paper published in the journal Science Translational Medicine today, lead authors Michael Farzan, PhD, and Mathew Gardner, PhD, describe their destruction of the “death star” strain and another especially hard-to-fight strain, suggesting it may be possible to protect uninfected individuals from multiple forms of HIV.
Their nontraditional vaccine achieved another critical goal: durability. This means it protected the research animals from infection long-term, with a single inoculation, Farzan says.
“We have solved two problems that have plagued HIV vaccine studies to date—namely, the absence of duration of response and the absence of breadth of response,” Farzan says. “No other vaccine, antibody or biologic protects against the two viruses for which we have demonstrated robust protection.”
Globally, about 180,000 new HIV infections occur in children annually, according to UNAIDS, and about 1 million people a year die of HIV/AIDS-related illnesses. Developing an HIV vaccine that protects long-term with a single dose is an important goal, especially in places where medical resources can be scarce, anti-retroviral drugs may be unavailable, and the risk of mother-to-infant transmission of HIV can be high.
The Farzan group’s work adds to the significant mark that Scripps Research is making in the fight against HIV. On July 10, the institute announced that the Scripps Consortium for HIV/AIDS Vaccine Development (CHAVD), an international collaboration led by Scripps Research, been awarded a $129 million, seven-year award from the National Institutes of Health to advance next-generation vaccines.Conventional vaccine approaches typically use a piece of virus or other immunogen to activate an immune system response. Because HIV replicates and changes so quickly, that approach has proven challenging. Farzan’s approach uses a safe virus to fight the dangerous one, and relies on muscle cells rather than immune cells to generate protective agents. Here’s how: A harmless, lab-made adeno-associated virus (AAV) carries within it a protective protein designed by Farzan and colleagues to stop HIV infectivity.
Called eCD4-Ig, the protective protein features two HIV co-receptors, CD4 and CCR5. The latter was discovered by Farzan and his team over a decade ago. Farzan’s viral vaccine is injected into muscle. It “infects” the muscle cells, which causes them to produce the protective eCD4-Ig. During exposure to HIV, the HIV virus is attracted to eCD4-Ig. It binds, and then “undergoes conformational change prematurely, and it’s no longer able to infect,” Farzan says.
The tough-to-stop research strain is SIVmac239, dubbed the “death star” because it has proven nearly impossible to defend against. It’s a type of simian immunodeficiency virus, which is an HIV-like virus that can infect primates. Primates are the only animals, other than humans, that support replication of these viruses.
There’s much more work to be done, notes first author Gardner. The study showed that the research animals could eventually become infected when exposed to atypically large loads of HIV. It also showed that HIV is capable of developing resistance to eCD4-Ig, albeit in a much-weakened state.
Encouragingly, the research animals did not develop serious immune reactions to the adeno-associated viral vector or the eCD4-Ig. Farzan said they had made concerted efforts to minimize that risk.
The use of AAV as a gene therapy tool has generated considerable excitement recently, gaining FDA approval for genetic diseases including inherited retinal disease and spinal muscular atrophy. This study shows it also has the potential save lives used as a protective vaccine, Farzan says.
“The results of our paper are encouraging for the potential of AAV as a platform for prevention of disease generally, and in concert with eCD4 as an agent for stopping HIV infection,” Farzan says. “We hope ultimately to prove that our approach is safe for both infected and at-risk persons at a cost that makes it useable everywhere.”
In addition to Farzan and Gardner, the authors of “AAV-delivered eCD4-Ig protects rhesus macaques from high-dose SIVmac239 challenges,” include: Co-first author Christoph H. Fellinger and Meredith E. Davis-Gardner, Jesse A. Weber, Barnett Alfant, Amber S. Zhou, Neha R. Prasad as well as Hema R. Kondur, all of the Scripps Research Department of Immunology and Microbiology in Jupiter, Florida. Other authors include Lisa M. Kattenhorn of Harvard Medical School Department of Microbiology and Immunology; Wendy A. Newton, Kim L. Weisgrau, Eva G. Rakasz and Nancy Schultz-Darken of the Wisconsin National Primate Research Center; Jeffrey D. Lifson of the AIDS and Cancer Virus Program at the Frederick National Laboratory for Cancer Research, and Guangping Gao of the University of Massachusetts Medical School’s Horae Gene Therapy Center and Department of Microbiology and Physiological Systems.
This project was supported by National Institutes of Health grants R01 AI080324 (M.F.), UM1 AI126623 (M.F., defeatHIV Delaney Cure Collaboratory), P01 AI100263 (G.G., M.F.) and F32AI122980 (M.R.G.), and by the Bill and Melinda Gates Foundation OPP1132169 (M.F.). M.R.G. is a recipient of the NIH Loan Repayment Program award. J.D.L. is supported in part with federal funds from the National Cancer Institute, National Institutes of Health, under contract HHSN261200800001E. Research reported in this publication was supported in part by the Office of the Director, National Institutes of Health under Award Number P51OD011106 to the Wisconsin National Primate Research Center, University of Wisconsin-Madison. This research was conducted in part at a facility constructed with support from Research Facilities Improvement Program grant numbers RR15459-01 and RR020141-01.
For more information, contact press@scripps.edu

