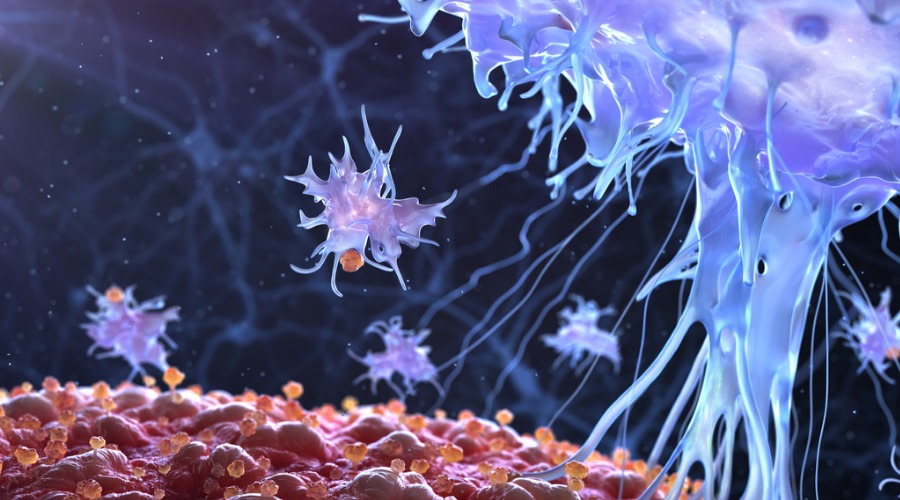
In new research, scientists from Scripps Research show that a protein called interleukin-27, or IL-27, is able to boost the body’s production of an especially beneficial type of self-renewing killer T cell. The knowledge may help inform the development of better cancer treatments.
Killer T cells that amplify immune response to viral infections may be a key to better cancer drugs
Scripps Research scientists discover a mechanism for promoting the proliferation of self-renewing T cells, offering a potential new pathway for enhancing cancer immunotherapy.
June 04, 2019
Scientists at Scripps Research have found a way to ramp up the body’s production of an especially powerful type of disease-fighting immune cell, offering a potential new avenue to create more effective cancer therapies that work across larger patient populations.
In recent years, new cancer immunotherapies known as PD-1 and PD-L1 inhibitors have become the standard of care for treating many different forms of cancer, from melanoma to bladder cancers. These “checkpoint inhibitor” drugs work by blocking proteins that would otherwise stop the immune system from attacking cancer cells.
But these groundbreaking drugs, while effective for some patients, don’t work for everyone.
Those who do respond tend to have something in common: Their bodies unleash a surge of killer T cells, also called CD8+ cells, which play an important role in targeting cancer tumors and helping the body fight back against viral infections.
However, over the course of disease, these cells can become exhausted and die off. Patients without a sustained response of these T cells are often unable to overcome their disease.
In a new study out of Scripps Research, published in the Journal of Experimental Medicine, researchers turned their focus to a distinct type of self-renewing killer T cells known as “CXCR5+ TIM3-” or “PD-1-responsive” that are unique in their ability to maintain their response during a persistent infection and proliferate after treatment with PD-1 checkpoint inhibitors.
Notably, scientists found that a protein called interleukin-27, or IL-27, is able to boost the body’s production of these ultra-beneficial T cells and prevent them from dying off in the face of disease. IL-27 is a protein in the family of cytokines, which are molecules that cells secrete to communicate with other cells.
“Previously, only cytokines that restrain these types of T cells were known, so it was exciting to find a pathway promoting T cell self-renewal in a chronic infection model,” says John Teijaro, PhD, assistant professor in the Department of Immunology and Microbiology at Scripps Research. “Our work revealed that the cytokine IL-27 protects CXCR5+TIM3- cells from death and helps them proliferate.”
Zhe Huang, PhD, postdoctoral fellow in Teijaro’s lab and a first author of the study, says that increasing IL-27 production and/or signaling may improve response to checkpoint blockade in human cancer patients. He notes that enhanced IL-27 signaling might also be useful in driving out persistent viruses such as human immunodeficiency virus (HIV) or hepatitis C, for which eliminating all infected cells remains a challenge.
“Unlike acute infections, overcoming chronic infections and cancer requires a sustained T cell response,” adds co-first author Jerry Zak, PhD, also a postdoctoral fellow in Teijaro’s lab at Scripps Research. “That means a continued survival and proliferation of those T cells that specifically recognize the infected or cancerous cells. Our experiments showed that protecting these T cells from excessive inflammation is not enough; they also need positive signals from IL-27 to keep dividing and stay alive.”
Looking ahead, Teijaro and his team would like to apply the study’s findings to clinical practice. Now that he knows how PD-1-responsive T cells are regulated, he’d like to determine whether treating patients with a combination of IL-27 and checkpoint blockades would create more powerful results. His lab also will seek easier ways to manipulate this pathway to regulate the numbers and function of these cells, such as with medicines that can be taken orally.
Besides validating the synergy of IL-27 with anti-PD-1/PD-L1 immunotherapy, they hope to identify cell types that produce IL-27. Uncovering how these cells are regulated will provide the knowledge base to generate new strategies for immunotherapy.
In addition to Teijaro, Huang and Zak, authors of the study, “IL-27 promotes the expansion of self-renewing CD8+ T cells in persistent viral infection,” include Isaraphorn Pratumchai of Scripps Research and Leiden University Medical Center; Namir Shaabani of Scripps Research, Vincent F. Vartabedian of Scripps Research; Nhan Nguyen of Scripps Research; Tuoqi Wu of the National Human Genome Research Institute; and Changchun Xiao of Scripps Research.
This work was supported by National Institutes of Health grants R01 AI118862 and R01 AI123210 (to J.R. Teijaro) and R01 AI121155 and R21 AI143529 (to C. Xiao).
For more information, contact press@scripps.edu

