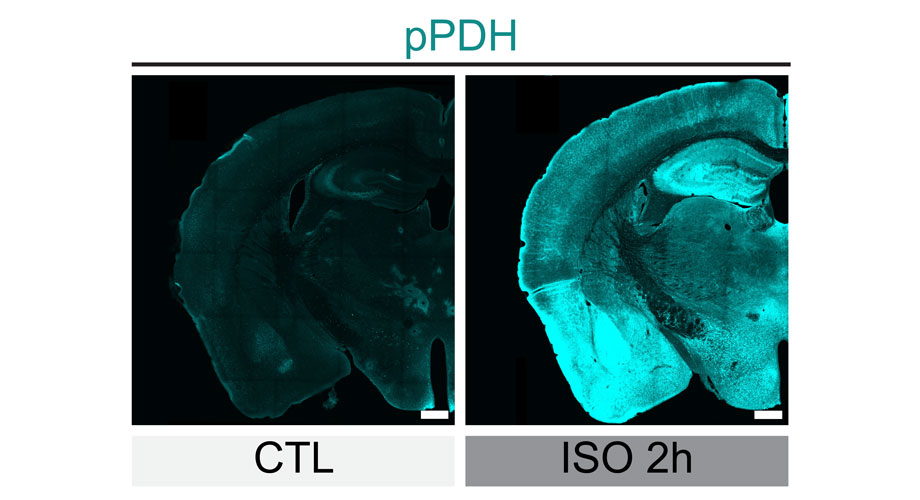
Levels of phosphorylated PDH (green) drastically increased in mouse brains cells after the mice were anesthetized for two hours (on right), showing the inhibition of the neurons. Credit: Scripps Research
New technology lets researchers track brain cells’ “off switches”
The method could shed light on what goes awry in numerous brain conditions when neurons are correctly and incorrectly activated or inhibited.
January 23, 2024
LA JOLLA, CA—For decades, scientists have studied the intricate activity patterns in human and animal brains by observing when different groups of brain cells turn on. Equally important to understanding the brain and related diseases, however, is knowing how long those neurons stay active and when they turn off again.
Now, scientists at Scripps Research have developed a new technology that lets them track when, after a burst of activity, brain cells shut off—a process known as inhibition. The technique, published in Neuron on January 23, 2024, provides a new way to study not only the normal functioning of the brain, but how the brain’s “off switches” may go awry in normal behaviors as well as in diseases and disorders, including depression, post-traumatic stress disorder and Alzheimer’s disease.
“It’s generally agreed that the inhibition, of neurons is really the major way the brain is regulating activity,” says senior author Li Ye, PhD, professor and Abide-Vividion Chair at Scripps Research. “Scientists have been looking for a way to look at inhibition on a more trackable way, and until now, few had found it.”
For pioneering the new approach, Ye teamed up with John Yates, a professor of Molecular Medicine at Scripps Research. They wanted to study how brain cells changed when they were actively firing—emitting an electrical charge to pass messages to their neighbors—compared to when they were done firing. The scientists used optogenetics, in which cells’ activity can be controlled using light, to repeatedly activate and inhibit the cells. Then, they measured levels and characteristics of different proteins and their modifications. They identified that one protein, pyruvate dehydrogenase (PDH), was very rapidly changed immediately after brain cells were inhibited.
“When neurons are firing, you need a lot of energy, and this PDH protein is involved in producing that energy,” explains Ye. “But the brain really wants to conserve energy, so when a cell is done firing, we found that the brain rapidly shuts off the PDH protein. This happened much faster than anything else we saw in gene expression.”
To shut off PDH, the researchers found, cells add molecular tags called phosphates to the protein. Ye and his colleagues found antibodies that only recognized this inactive, phosphorylated form of PDH (pPDH). To test whether levels of phosphorylated PDH (or pPDH) could be used as a proxy for brain cell inhibition, Ye’s team used these antibodies to measure pPDH in mice that had been given anesthesia. Nearly the entire brain lit up with high levels of pPDH, correctly showing how most of the brain is inactive during anesthesia.
The group also studied levels of pPDH when animals were exposed to bright light that was then shut off. Brain cells in the visual cortex, responsible for vision, had low levels of pPDH when being exposed to light (because the active form of PDH would be required to give these cells signaling energy), but high levels of phosphorylated protein immediately increased after the light was off.
Ye’s group also used the new technique to study a less understood process: how the brain turns off the feeling of hunger after a meal. They showed how brain cells related to appetite shut off when a mouse starts to eat. Those findings could have implications for better understanding appetite, obesity and some weight loss drugs. More broadly, the pPDH antibodies could be used to compare levels of brain cell inhibition in healthy people and those with a variety of brain and metabolic diseases.
“There are a lot of questions that this technology can help us answer,” says Ye. “If the brain can’t turn cells off, or if they’re turned off faster or slower than usual, what happens? How does the inhibition of neurons play a role in different diseases?”
Ye and his colleagues are continuing to fine-tune the use of pPDH, but they say that other researchers are already using the technology—the antibodies used to measure pPDH are commercially available.
In addition to Ye and Yates, authors of the study, “Phosphorylation of pyruvate dehydrogenase inversely associates with neuronal activity,” include Dong Yang, Yu Wang, Tianbo Qi, Xi Zhang, Leyao Shen, Jingrui Ma, Zhengyuan Pang, Neeraj K. Lal, Daniel B. McClatchy, Saba Heydari Seradj, Verina H. Leung, Kristina Wang, Yi Xie, Filip S. Polli, Anton Maximov, Hollis T. Cline and Vineet Augustine of Scripps Research; and Oscar Christian Gonzalez and Luis de Lecea of Stanford University.
This work was supported by funding from the National Institutes of Health (DP2DK128800), and BRAIN initiative/NIMH (MH132570and the Dorris Scholar Award.
For more information, contact press@scripps.edu

