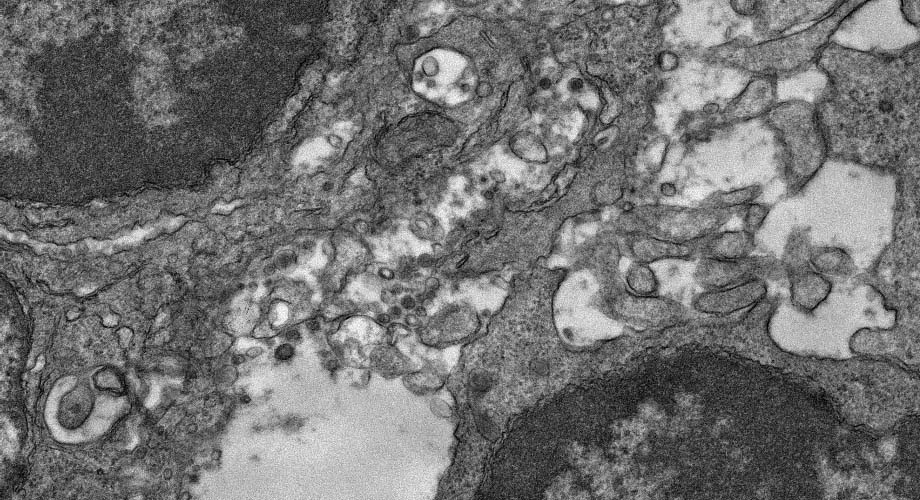
An electron microscopy image of lymph node tissue from a mouse that was immunized with an experimental COVID-19 vaccine. Vaccine particles are readily taken up by immune cells, stimulating antibody production for several weeks. (Image courtesy of Yi-Nan Zhang, Kimberly Vanderpool, Theresa Fassel and Scott Henderson.)
New SARS-CoV-2 vaccine candidate shows great promise against variants of concern
Study suggests the experimental vaccine may engage the immune system much more robustly than other vaccine strategies.
October 20, 2021
LA JOLLA, CA—A nanoparticle-based COVID-19 vaccine developed by scientists at Scripps Research elicited immune responses suggesting very potent and broad protection against SARS-CoV-2 in a preclinical study. The results need to be confirmed in human trials, but point to the possibility of achieving powerful and enduring immunity against all major SARS-CoV-2 variants.
The experimental vaccine, described in a paper in Science Advances, does not use viruses, messenger RNA, or loose copies of the SARS-CoV-2 spike protein, and instead is made from proteins that self-assemble into virus-like nanoparticle structures.
In mice, the researchers found, these nanoparticle structures elicit immune responses that powerfully neutralize the original Wuhan strain of SARS-CoV-2, and—with the same potency—all the other major variants of concern including the fast-spreading delta variant.
The scientists also examined the cellular roots of the immunity induced by their experimental vaccine, showing how its coronavirus-like particles—compared to the loose copies of the SARS-CoV-2 spike protein used by other vaccines—had much longer and stronger engagement with the immune cells that give rise to long-term immunity.
“These are very promising results, and other researchers in the vaccine field may want to consider adopting, as standard benchmarks for vaccine comparison, the measures of vaccine engagement with immune cells that we made in this study,” says study senior author Jiang Zhu, PhD, an associate professor in the Department of Integrative Structural and Computational Biology at Scripps Research.
The self-assembling nanoparticle design is one that Zhu and his colleagues have used in recent years for other candidate vaccines, including for HIV, hepatitis C virus, and Ebola virus. It features a nanoparticle sphere of protein into which smaller proteins that mimic the virus’s outer spike proteins embed themselves. The spike proteins used for the vaccine are more stable, and in that sense are thought to be better able to stimulate an immune response, than those found in the real virus and in those produced by current mRNA and virus-vector COVID-19 vaccines. The result is a structure that broadly resembles that of a real SARS-CoV-2 particle and powerfully stimulates an immune response against the virus—and yet, unlike some other protein vaccine concepts, is self-assembling and can be manufactured relatively easily on a large scale, Zhu says.
In March, Zhu and colleagues reported similarly encouraging early results from studies of this candidate vaccine, including the finding that the blood of mice immunized with it can neutralize not only SARS-CoV-2 but also its distant cousin the SARS-CoV-1 virus, which caused a serious outbreak mainly in East Asia in 2002-04.
In the new study, the researchers conducted a more extensive set of tests, including tests of the ability of antibody-containing blood plasma from immunized mice to neutralize different SARS-CoV-2 variants. The researchers found that the plasma could powerfully neutralize—blocking cell-to-cell infection in the lab dish—not only the SARS-CoV-2 “Wuhan” reference strain, but also, with equal effectiveness, the B.1.1.7 “alpha” variant that emerged in the UK, the B.1.351 “beta” variant that emerged in South Africa, the P.1 “gamma” variant that emerged in Brazil, and a version of the B.1.617 “delta” variant that emerged in India and remains as the fastest-spreading, most dominant variant.
Zhu and his team then isolated from immunized mice a set of specific antibodies that account for this broad neutralizing ability, and showed that a vaccine design based on loose spike proteins—like the current mRNA and virus-vector vaccines—induce antibodies of lesser neutralization breadth.
Finally, the researchers examined the biological process of immunity induction, showing with electron microscopy in the lymph nodes of immunized mice how their experimental vaccine particles engage with follicular dendritic cells—immune cells that gather and present viral particles to help start a robust immune response—as well as antibody-producing B cells. They compared this engagement with that of a loose spike protein design, and the results suggested, by various measures, that the new nanoparticle-based vaccine candidate is greatly superior in its ability to stimulate these immune elements. For example, nanoparticle-based vaccine particles were displayed four times as extensively on follicular dendritic cells, and stimulated much longer and larger B-cell responses known as germinal center reactions.
The study thus suggests that the nanoparticle-based design, if eventually approved for use after clinical trials—which Zhu hopes to begin next year—could greatly outperform other COVID-19 vaccines in terms of the potency of protection, the breadth of protection, and perhaps also the duration of protection.
Moreover, Zhu says, the studies his team conducted of the candidate vaccine’s ability to engage follicular dendritic cells and stimulate B cells, and to elicit spike-specific broadly neutralizing antibodies, suggest the wider use of such measures as standard benchmarks for evaluating experimental vaccines in preclinical tests.
“It would be a more uniform, evidence-based way of evaluating the promise of vaccine candidates early in development,” Zhu says.
“Mechanism of a COVID-19 nanoparticle vaccine candidate that elicits a broadly neutralizing antibody response to SARS-CoV-2 variants” was co-authored by Yi-Nan Zhang, Jennifer Paynter, Cindy Sou, Tatiana Fourfouris, Timothy Ngo, Linling He, and Jiang Zhu, all of Scripps Research; and by Ying Wang, Ciril Abraham, and Yi Zhang of Temple University.
The research was funded by the National Institutes of Health (AI137472, AI139092) and by Uvax Bio LLC.
For more information, contact press@scripps.edu

