Experimental COVID-19 vaccine takes novel approach to boosting immune response
The protein-based vaccine delivers particles that mimic the shape of a whole virus; early tests in mice suggest it also may work against variants of SARS-CoV-2.
March 19, 2021
LA JOLLA, CA—Scientists at Scripps Research have created an experimental COVID-19 vaccine that works differently than vaccines currently in use—and may provide some important advantages, according to the results of a new study.
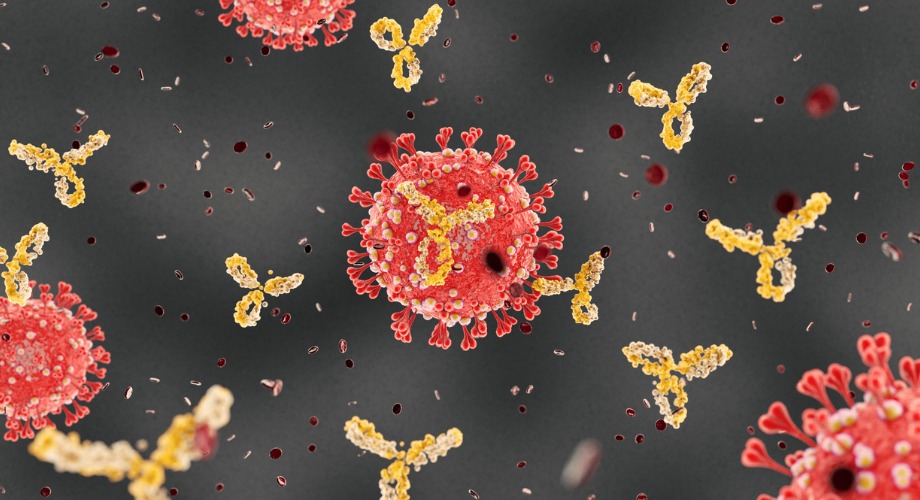
Unlike current COVID-19 vaccines that have gained emergency use authorization, which rely on RNA or viral DNA to instruct cells to create individual spike proteins from the virus, this approach presents the spike proteins on tiny spherical protein particles that more closely mimic the shape of the actual virus.
The goal is to trick the immune system into producing powerful and broad protection against COVID-19, says Jiang Zhu, PhD, associate professor in the Department of Integrative Structural and Computational Biology at Scripps Research.
In early tests in mice, the vaccine produced strong neutralizing antibody responses against the original SARS-CoV-2 strain (Wuhan-Hu-1) and provided some protection from the distantly related coronavirus SARS-CoV-1, which causes SARS. It also induced significant responses from T cells, which are another important component of immune protection from viruses. The findings appear in Science Advances.
“In mice, this protein-based vaccine produced a strong and broad immune response, which is exactly what we would want to see in a COVID-19 vaccine that protects against multiple variants,” says Zhu, who led the study.
The experimental vaccine is designed according to a concept that Zhu and colleagues have used in recent years to develop other vaccine candidates, including for HIV and hepatitis C. The resulting virus-like-particles are roughly the same size as a real virus particle, with similar surface-level structural organization.
The vaccine itself self-assembles during the biomanufacturing process, which should make large-scale production relatively easy, Zhu says.
Confronting the problem of spike stability
In developing the experimental vaccine, the team identified and addressed an issue that hasn’t been resolved in vaccines currently in use. The issue concerns the SARS-CoV-2 spike protein, which the virus uses to grapple to and enter cells during infection. On the virus surface, these spikes bend over to various degrees and form clusters, which, some scientists believe, is related to variations in quality of antibody response seen in COVID-19 patients.
To improve the immune response over what might naturally occur from COVID-19 infection, most current vaccines prompt cells to create a full-length but slightly mutated version of the spike protein, known as the S2P version, which is designed to be more stable. However, after the current vaccines were created, several laboratories reported—and Zhu and his team also observed—that this standard spike design may not stimulate the best-possible immune response due to certain differences in structural properties caused by the stabilizing mutations.
Zhu and colleagues altered the spike protein in a different way for their vaccine candidate and showed in the study that it was more stable than a soluble form of the S2P spike (which is similar, but not exactly the same, as the full-length spike created by vaccines). In mice, the new version of the spikes elicited twice the level of neutralizing antibodies compared with the soluble S2P spike. And when the new spikes were mounted in large numbers on virus-like particles, performance improved even further: they elicited up to 10 times the level of neutralizing antibodies compared with the soluble S2P spikes.
The spike-studded particles also induced T cell responses, suggesting protection from the powerful T cell arm of the immune system.
Protection beyond COVID-19?
When the researchers tested the blood of mice that had been inoculated with the virus-like particles, they also found high levels of antibodies capable of neutralizing SARS-CoV-1—the original SARS coronavirus, which caused deadly outbreaks in Hong Kong, South China, Canada and a few other areas nearly two decades ago.
Both SARS-CoV-1 and SARS-CoV-2 are believed to have originated as bat-infecting coronaviruses, but they are only about 70 percent identical in the crucial viral structure known as the “receptor-binding domain,” which enables the spike proteins to attach to human cells.
“The ability of this experimental vaccine to elicit neutralizing antibodies against the coronaviruses that cause COVID-19 and SARS is promising and warrants further investigation,” Zhu says.
Zhu and his colleagues are now conducting more advanced experiments that they hope will enable them to test their approach in early-stage clinical trials, pending the FDA’s approval.
“Single-component, self-assembling, protein nanoparticles presenting the receptor binding domain and stabilized spike as SARS-CoV-2 vaccine candidates” was co-authored by Linling He, Xiaohe Lin, Ying Wang, Ciril Abraham, Cindy Sou, Timothy Ngo, Yi Zhang, Ian Wilson and Jiang Zhu.
Support was provided by grants from the National Institutes of Health (AI129698, AI140844) and Uvax Bio LLC, a vaccine development company co-founded by Zhu.
For more information, contact press@scripps.edu

