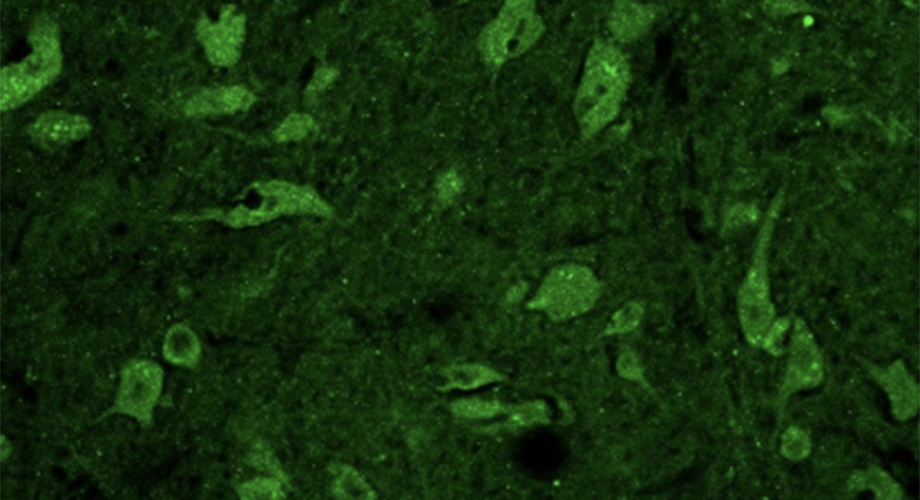
Photo caption: Mouse neurons and glial cells are stained to show degeneration from ribosome quality control mutations. (Credit Haifei Xu, Joazeiro lab, Scripps Research, Florida.)
New gene implicated in neuron diseases
A defective protein quality control system leads to motor neuron death, as seen in disorders such as ALS.
September 16, 2020
JUPITER, FL — Failures in a quality control system that protects protein-building fidelity in cells can lead to motor neuron degeneration and related diseases, according to a new study from an international team co-directed by Scripps Research molecular biologist Claudio Joazeiro, PhD.

Scripps Research Molecular Medicine Professor Claudio Joazeiro, PhD.
Motor neurons control movement, breathing, swallowing and speaking. Their death is a hallmark of progressive diseases such as spinal muscular atrophy and ALS, also known as Lou Gehrig’s disease. Understanding what can cause motor neurons to die is a key to developing precision treatments. Scientists are finding that the causes of motor neuron diseases are many.
The study, appearing in the journal Nature Communications, singles out several variants of a gene called NEMF as a new driver of motor neuron diseases. NEMF, short for “nuclear export mediator factor,” is known for its role in helping clear glitches that inevitably occur during protein production by cellular organelles called ribosomes.
Healthy NEMF helps the cell recycle garbled protein fragments produced in error. But several mutant forms of NEMF in mice interfered with the system and resulted in neuromuscular, neurodegenerative or other disease, the scientists found.
The research was led by both Joazeiro, who has joint appointments at Scripps Research in Jupiter, Florida and the Center for Molecular Biology of Heidelberg University in Germany, and Gregory Cox, PhD, of the Jackson Laboratory of Mammalian Genetics in Bar Harbor, Maine.
A decade ago, Joazeiro discovered an enzyme, the E3 ubiquitin ligase listerin/Ltn1, that works in a specialized quality control process now known as RQC, or ribosome-associated quality control. He and his team also found that inactivation of the enzyme causes motor neuron degeneration in mice. However, whether neurodegeneration resulted from defective ribosome-associated quality control or some other function of listerin, remained unclear. At the Jackson Laboratory, Cox had been studying mice with mutations in another quality control factor, NEMF. They exhibited movement difficulties including walking and gripping. The labs teamed up to investigate whether those defects resulted from a neurodegenerative process. They wanted to find the molecular mechanisms at work.
“The results provide strong evidence that dysfunction of ribosomal quality control causes neurodegeneration,” Joazeiro says.
Within cells, millions of ribosomes transform genetic code into proteins by stringing together one amino acid at a time. Mistakes occasionally happen, some of which lead to the production of potentially toxic protein fragments. When that happens, manufacturing may be suspended, and the cell’s ribosome protein quality control system chops up the garbled pieces for recycling.
But whether defective ribosome quality control contributed to human disease had remained unknown. Human data backed up the team’s mouse and yeast-based investigations.
Working through GeneMatcher, a tool for patients developed at the Baylor-Hopkins Center for Mendelian Genomics in Texas, the team identified nine patients from seven unrelated families who had likely pathogenic NEMF variants and displayed neuromuscular disease, along with a variety of developmental issues including speech delay and intellectual disability.
“It was amazing to see how our early and new mouse data, together with the knowledge acquired on molecular mechanisms, were so predictive of these findings in human patients,” Joazeiro says. “We’re hopeful these advances will one day prove helpful to families affected by these difficult diseases.”
The team is now investigating the role of ribosome-associated quality control in other related diseases, he adds.
Another fascinating takeaway from this research is that this pathway of protein quality control appears to be necessary across species, he adds.
“Last year we reported that it is also present in bacteria, and is likely to have already been active in the last universal common ancestor, the organism that gave rise to all domains of life,” Joazeiro says.
Together with the findings that disabling the system results in neurodegeneration, this evolutionary conservation highlights the importance of aberrant protein disposal, and also suggests the system’s development may have played a critical role enabling the evolution of complex organisms, Joazeiro says.
“This research shows that failure of ribosome-associated quality control is a cause of motor neuron disease that should be explored in greater detail,” he says.
In addition to lead co-authors Joazeiro and Cox, contributors to the study, “NEMF mutations that impair ribosome-associated quality control are associated with neuromuscular disease,” include co-first authors Paige B. Martin of the Jackson Laboratory of Mammalian Genetics in Bar Harbor, Maine and the University of Maine, and Yu Kigoshi-Tansho of the Center for Molecular Biology of Heidelberg University. Additional authors are: Ryo Yonashiro and Tina Müller of Scripps Research, Florida; Jennifer Stauffer of the Jackson Laboratory of Mammalian Genetics; Rajesh Kumar of Heidelberg University; Roger Sher of Stony Brook University; Gianina Ravenscroft, Denise Howting and Nigel Laing of the University of Western Australia; Christopher Griffith of the University of South Florida College of Medicine; William Allen of the Mission Fullerton Genetics Center; Davut Pehlivan, Jennifer E. Posey and James Lupski of the Baylor College of Medicine; Tamar Haral of Hadassah-Hebrew University Medical Center; Martin Zenker and Denny Schanze of the Institute of Human Genetics, Otto-von-Guericke University, Magdeburg; Eissa A. Faqeih of the Department of Genetics, King Fahad Medical City; Naif A. M. Almontashiri of Taibah University; Reza Maroofian and Henry Houlden of the Neurogenetics Laboratory, UCL Queen Square Institute of Neurology and the National Hospital for Neurology and Neurosurgery, London; Neda Mazaheri and Hamid Galehdari of Shahid Chamran University of Ahvaz, Iran; Ganka Douglas of GeneDx, Inc.; and Monique Ryan of the Royal Children’s Hospital, Melbourne, Murdoch Children’s Research Institute and University of Melbourne.
The work was supported by the National Institutes of Health, (R01 NS102414 and R01 NS075719) the National Institute of Neurologic Disorder and Stroke (R35 NS105078) and the National Human Genome Research Institute (K08 HG008986). It was also supported by the Baylor Hopkins Center for Mendelian Genomics (UM1 HG006542), and ALS Association grant (16-IIP-287) and a Clinical Research Training Scholarship in Neuromuscular Disease partnered by the American Brain Foundation and Muscle Study Group.
For more information, contact press@scripps.edu

