Regenerative Chemical Turns Muscle Cells into Stem Cells
By Jason Socrates
Bardi
A group of researchers from The Scripps Research Institute
has identified a small synthetic molecule that can induce
a cell to undergo dedifferentiation—to move backwards
developmentally from its current state to form its own precursor
cell.
This compound, named reversine, causes cells which are normally
programmed to form muscles to undergo reverse differentiation—retreat
along their differentiation pathway and turn into precursor
cells. These precursor cells are multipotent; that is, they
have the potential to become different cell types. Thus, reversine
represents a potentially useful tool for generating unlimited
supply of such precursors, which subsequently can be converted
to other cell types, such as bone or cartilage.
"This [type of approach] has the potential to make stem
cell research more practical," says Sheng Ding. "This will
allow you to derive stem-like cells from your own mature cells,
avoiding the technical and ethical issues associated with
embryonic stem cells."
Ding, who is an assistant professor in the chemistry department
at Scripps Research conducted the study—to be published
in an upcoming issue of the Journal of the American Chemical
Society—with Peter G. Schultz, who is a professor
of chemistry and Scripps Family Chair of Scripps Research's
Skaggs Institute of Chemical Biology, and their colleagues.
Regenerative Medicine and Stem Cell Therapy
Stem cells have huge potential in medicine because they
have the ability to differentiate into many different cell
types—potentially providing doctors with the ability
to produce cells that have been permanently lost by a patient.
For instance, the damage of neurodegenerative diseases like
Parkinson's, in which dopaminergic neurons in the brain are
lost, may be ameliorated by regenerating neurons. Another
example of a potential medical application is Type 1 diabetes,
an autoimmune condition in which pancreatic islet cells are
destroyed by the body's immune system. Because stem cells
have the power to differentiate into islet cells, stem cell
therapy could potentially cure this chronic condition. However
bright this promise, many barriers must be overcome before
stem cells can be used in medicine. Stem cell therapy would
be most effective if you could use your own stem cells, since
using one's own cells would avoid potential complications
from immune rejection of foreign cells. However, in general
it has proven very difficult to isolate and propagate stem
cells from adults. Embryonic stem cells (ESCs) offer an alternative,
but face both practical and ethical hurdles associated with
the source of cells as well as methods for controlling the
differentiation of ESCs. A third approach is to use one's
own specialized cells and dedifferentiate them.
Normally, cells develop along a pathway of increasing specialization.
Muscles, for instance, develop after embryonic stem cells
develop into "mesenchymal" progenitor cells, which then develop
into "myogenic" cells. These muscle cells fuse and form the
fibrous bundles we know as muscles.
In humans and other mammals, these developmental events
are irreversible, and in this sense, cell development resembles
a family tree. One wouldn't expect a muscle cell to develop
into a progenitor cell any more than one would expect a woman
to give birth to her own mother.
However, such phenomena do happen in nature from time to
time.
Some amphibians have the ability to regenerate body parts
that are severed by using dedifferentiation. When the unlucky
amphibian loses a limb or its tail, the cells at the site
of the wound will undergo dedifferentiation and form progenitor
cells, which will then multiply and redifferentiate into specialized
cells as they form an identical replacement to the missing
limb or tail. In humans, the liver is unique in its regenerative
capacity, possibly also involving dedifferentiation mechanism.
The Scripps Research scientists hope to find ways of mimicking
this natural regeneration by finding chemicals that will allow
them to develop efficient dedifferentiation processes whereby
healthy, abundant, and easily accessible adult cells could
be used to generate stem-like precursor cells, from which
they could make different types of functional cells for repair
of damaged tissues. Reversine is one of the first steps in
this process.
However, tissue regeneration is years away at best, and
at the moment, Schultz and Ding are still working on understanding
the exact biochemical mechanism whereby reversine causes the
muscle cells to dedifferentiate into their progenitors, as
well as attempting to improve the efficiency of the process.
"This [type of research] may ultimately facilitate development
of small molecule therapeutics for stimulating the body's
own regeneration," says Ding. "They are the future of regenerative
medicine."
The article, "Dedifferentiation of Lineage-Committed Cells
by a Small Molecule" is authored by Shuibing Chen, Qisheng
Zhang, Xu Wu, Peter G. Schultz, and Sheng Ding and is available
to online subscribers of the Journal of the American Chemical
Society at: http://pubs.acs.org/cgi-bin/asap.cgi/jacsat/asap/html/ja037390k.html.
The article will also be published in an upcoming issue of
JACS.
This work was supported by The Skaggs Institute for Research
and the Novartis Research Foundation.

|
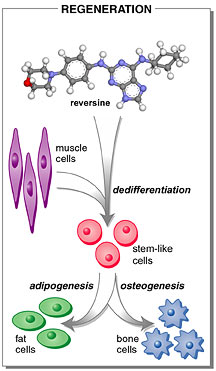
The synthetic chemical reversine induces
dedifferentiation, which is the key process of epimorphic
regeneration in nature—when a lost limb, for instance,
grows back in the same form. Picture
courtesy of Sheng Ding.
|

