

New Lupus Drug Results from Scripps Research Technology
By Mika Ono and Mark Schrope
Scientific advances at The Scripps Research Institute were key to laying the foundation for the new drug Benlysta® (belimumab), approved March 9, 2011, by the U.S. Food and Drug Administration. Benlysta®, which treats the most common type of lupus, is the first in a new class of pharmaceuticals that prevents the body from attacking its own critical tissues.
"I am deeply gratified that our scientific findings have proven so valuable to drug discovery," said Richard A. Lerner, president of Scripps Research. "This development underlines the importance of basic academic science in laying important groundwork for life-saving medical advances."
Benlysta®, developed by GlaxoSmithKline and Human Genome Sciences, is the first new drug treatment for lupus in 50 years.
Short-Circuiting the Cycle of Lupus
Benlysta® was approved for systemic lupus erythematosus, a chronic, life-threatening inflammatory disease affecting the joints, skin, kidneys, blood, heart, and lungs. It is often simply referred to as "lupus" (although there are other types of lupus, including one that affects solely the skin). Estimates of the number of Americans affected by sytemic lupus erythematosus range from 161,000 to 1.5 million, according to the U.S. Centers for Disease Control. Lupus can occur at any age, but first appears largely in 15- to 40-year-olds, the majority of whom are women.
Lupus is an autoimmune disease, which occurs when a person's body produces an immune response against its own tissues instead of solely attacking foreign invaders such as viruses, bacteria, and other toxins.
Symptoms can include debilitating fatigue, painful and swollen joints, fever, skin rash, and kidney problems. The disease can also lead to arthritis, kidney failure, heart and lung inflammation, central nervous system abnormalities, inflammation of the blood vessels, and blood disorders.
Benlysta® (itself a type of immune molecule) acts by targeting a specific protein called B-lymphocyte stimulator, or BLyS, involved in stimulating the "autoantibodies" causing lupus and certain other autoimmune disorders.
Benlysta® is the first approved drug that disables BLyS, thus preventing the immune system's destructive attacks against the body.
The Foundation
In the 1980s the therapeutic potential of antibodies—which recognize a wide range of foreign pathogens, then alert the immune system to the presence of the invaders—was widely recognized, as they are an important part of the body's natural system for fighting illness. But tapping that potential had proven difficult. Researchers at the time were working mainly with short snippets of antibodies and testing their effects through a slow and painstaking petri-dish process.
But Lerner led a Scripps Research team that made two critical advances to transform the field, ultimately leading to the discovery and development of drugs such as Benlysta®.
The researchers first developed a method of combining different pieces of antibodies isolated from human or animal cells into proteins long enough to encompass natural antibodies' most critical portions—the parts actually binding to and neutralizing infectious agents or otherwise unwanted material. The scientists dubbed this technique "repertoire cloning," because it allowed them to build libraries of compounds that encompassed the full repertoire of a natural immune system.
This was a game-changing development.
Eliminating the Petri-Dish Bottleneck
But even with an expansive repertoire, putting it to use was a separate problem. It was a second key Scripps Research discovery that helped eliminate the petri-dish bottleneck.
In the 1989 to 1991 timeframe, Lerner and his colleagues pioneered a technique for employing phage display to facilitate large "combinatorial antibody libraries" to find human antibodies that could be used therapeutically.
Combinatorial antibody libraries allow human antibodies to be identified directly by searching among billions of antibody variants taken from human blood samples to find those that bind to a particular target—such as BLyS—involved in a particular disease.
In this technique, the scientists hijack the inner workings of phages (viruses that attack bacteria). By inserting genetic sequences encoding active portions of antibodies, the researchers are able to make phages displaying on their surfaces the antibody of interest. These antibody-displaying phage particles can then be tested en masse for their ability to bind to molecules of interest. Successful binders can then be purified and identified as a target for additional research.
With the British Medical Research Council (MRC) Laboratory of Molecular Biology, Scripps Research licensed the inventions to Cambridge Antibody Technology (now part of AstraZeneca) to facilitate exploitation of the technology for creation of new medicines. In 1999, Cambridge Antibody Technology partnered with Human Genome Sciences, which entered into a co-development and commercialization agreement with GlaxoSmithKline in 2006.
While much technology has changed over the decades, variations of combinatorial antibody libraries are still a mainstay of drug discovery research. Commercialized throughout the 1990s, the promise of this method is now beginning to be realized—today with Benlysta®, tomorrow, Lerner predicts, with other life-saving drugs.
Send comments to: mikaono[at]scripps.edu
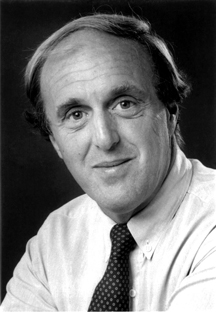
"I am deeply gratified that our scientific findings have proven so valuable to drug discovery," said Richard A. Lerner, president of Scripps Research.
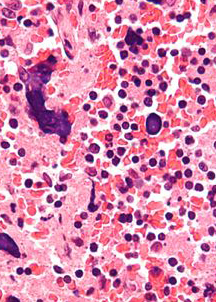
Technology from the Lerner lab made possible the development of Benlysta®, recently approved to treat systemic lupus erythematosus, a chronic, life-threatening inflammatory disease. This image shows disease-related changes to a lymph node. (Image by Nephron, GNU Free Documentation)
