

Scripps Research Team Makes First Cell Culture System for Hepatitis C Virus
A Tool for Advancing Vaccine, Drug Research
By Jason Socrates Bardi
In a surprising first, a group of researchers led by scientists at The Scripps Research Institute has developed a way to create a robust infection of liver cells with one strain of hepatitis C virus in vitro. The researchers can grow the cells in the appropriate conditions, infect them with the hepatitis C virus, collect new virus particles as the virus replicates, and go on to infect more cells—essentially replicating exactly what the hepatitis C virus does in the liver of infected patients.
Why this be considered an important step?
"Because," says Scripps Research Professor Francis V. Chisari. "It's a great system to use to study the viral life-cycle and to look for drugs that can block the virus in different stages of that life-cycle.
Chisari led the research with Scripps Research Associates Jin Zhong, Pablo Gastaminza, Guofeng Cheng, and Sharookh Kapadia. A paper describing the results is to be published in an upcoming issue of the journal Proceedings of the National Academy of Sciences.
An effective vaccine against hepatitis C virus would be a huge boon. Currently, there is no vaccine against the disease, which is one of the most common blood-borne infections in the world today. According to the U.S. Centers for Disease Control and Prevention (CDC), hepatitis C virus currently infects some 3.9 million Americans and more than 180 million people worldwide. An additional 30,000 or so people are infected each year in the United States.
New drugs to treat people who have already contracted hepatitis C would also be of great benefit since hepatitis C virus is also one of the most common causes of chronic liver disease in the United States and is the number one indication leading to liver transplantation. About 75 percent of people infected with the virus are chronically infected, which in time leads to scarring of the liver, impaired liver function, cirrhosis of the liver, and a greatly enhanced predisposition to developing liver cancer.
"The lifecycle of the virus is now completely open to us," says Chisari. "There is a lot of optimism [in the field] that we will be able to develop better, targeted therapeutic drugs against hepatitis C virus."
Hepatitis C—A Nasty and Often Deadly Infection
Hepatitis is a disease caused by one of several evolutionarily distinct viruses (called A, B, C, D and E). Hepatitis C virus is a linear, single-stranded RNA virus about 10,000 base pairs long that targets cells of the liver.
The virus is passed from person to person through direct contact of bodily fluids—most often through exposure to infected blood. Many of the people who are infected with hepatitis C virus today received blood transfusions, organ transplants, or blood products prior to the late 1980s, when good diagnostics for screening out hepatitis-infected blood became available.
Even so, tens of thousands of people are exposed to the virus each year in the United States, and it continues to spread through contaminated needles, mother-to-infant transmission, and unprotected sex, though the risk of transmission is lower than other sexually transmitted diseases. There are even rare cases where people have contracted hepatitis C virus from dental work, acupuncture, tattooing, and body piercing.
The virus enters the bloodstream packaged into an infectious particle, or virion, that's about 50 nanometers in diameter (about 10,000 times smaller that the period at the end of this sentence). No structure of the virion exists, but scientists know that it has a protein capsid shell surrounded by a lipid coat.
Once inside the bloodstream, the virus particles circulate through the blood until they reach the liver, where they enter hepatocytes, the tiny chemical factories in the liver that produce most of the proteins present in blood, nurturing all the other organs of the body. They also produce bile, a fluid used for the digestion of fat in the diet and for the elimination of waste.
The hepatitis C virus sets up shop inside the hepatocyte and begins to make copies of itself, using its own imported enzymes and a number of the liver cell's own proteins. The viral genome is a "plus" strand of RNA that is translated by the ribosome to produce a large polyprotein that is cleaved by cellular proteases to produce the individual viral proteins. One of those proteins is an RNA "polymerase" enzyme that copies the plus-strand RNA into many minus-strands. The minus strands are then copied back into many more plus strands, thereby amplifying the amount of viral RNA in the cell. Finally, new virions are assembled and exported from the cell where they can infect new cells and, thus, start the cycle all over again.
The initial number of cells infected may be small—just a few—but within six to eight weeks, the infection has spread, and the virus can infect every hepatocyte cell in the liver. This is remarkable given that the liver is such a large organ, containing somewhere on the order of 100 billion cells.
Upon widespread infection, viral RNA in the bloodstream spikes rapidly, which elicits an immune response. Cells infected with the virus display pieces of the virus—antigen—on their surface. The immune system selects specialized cells called cytotoxic T lymphocytes or "killer T cells" for their ability to recognize pieces of the virus, and the killer T cells expand into a clone army of cells all gunning for cells displaying that antigen. These killer T cells begin killing off infected liver cells, reducing by several orders of magnitude the amount of virus in the blood.
Some adults with hepatitis C suffer an acute infection, in which the body mounts an immune response so effective that the virus disappears. However, in about three-quarters of all people with hepatitis C virus—about 2.7 million people in the United States—the immune response is not sufficient to completely wipe out the virus, and the infection turns chronic.
Chronic Hepatitis, Liver Disease, and Therapy
Chronic hepatitis is a smoldering infection, and for reasons that are not entirely clear the body fails to mount an immune response that is sufficiently strong to completely clear the virus from the liver. This sets up a scenario somewhat like those coal mine fires that have been burning in Pennsylvania for years—the fire will burn itself out in one part of the mine, and then a new shaft will open up, feed the fire, and start some other part of the tunnels burning. In a chronic hepatitis C infection, as the cells in the liver are killed, new liver cells are generated, and these become infected as well.
The immune system attempts to keep this continual infection in check, and this leads to a slow, progressive process in which the killer T cells destroy some of the infected hepatocytes, others are infected, the T cells kill those, the liver grows more, they are infected, and the killer T cells continue killing. In chronically infected individuals, the virus infects new cells in the liver even as the immune systems kills off already infected cells.
This cumulative destruction can ultimately lead to fibrosis or scarring of the liver, which is serious because the scar tissue impedes blood flow. The decreased blood flow can then cause a number of other complications, including jaundice, which can be seen as a yellow coloring of the eyes and skin because of the release of bile into the bloodstream.
"All those processes combined are described as cirrhosis of the liver, and when it is severe, it leads to the failure of the liver to perform its detoxification and synthetic [roles]," says Chisari. "This terribly compromises the function of the liver and shortens the life of the patient."
Even if chronically infected patients don't succumb to cirrhosis, they can fall victim to the virus in another way, through cancer of the liver. Cancer is much more likely to occur in chronically infected patients because the liver cells often undergo rapid turnover during an infection, increasing the probability of random point mutations accumulating in the DNA of those cells.
"[People with chronic hepatitis] have a 100- to 200-fold increased risk for developing liver cancer," says Chisari. "By comparison, heavy smokers have only a 10-fold higher risk of developing lung cancer."
Hepatitis C is also a major contributor to other diseases as well, complicating, for instance, the health of people who are coinfected with pathogens such as human immunodeficiency virus (HIV).
Like HIV, the hepatitis C virus has a high rate of replication and is also prone to mutation during replication. Because of the virus's ability to mutate, a single drug monotherapy is not effective because mutants resistant to that drug can readily arise.
Multiple drugs are needed to minimize this risk, and the current treatment of choice for hepatitis C patients is a combination of the inflammatory chemical interferon-alpha with the antiviral drug ribavirin. This combination is successful at reducing the viral load in about 40 to 80 percent of cases, but it is not effective in all people—especially those infected with certain strains of the virus, such as those that predominate in the United States.
Even if the interferon/ribavirin treatment is effective for an individual, its use is complicated by a number of other factors, including its cost, the tolerance of the drug by the patient, and the fact that treatment can be toxic. Interferon produces flu-like symptoms after a person is injected—usually a few times a week for about 6 months, says Chisari. Plus, the drug has the side-effect of causing clinical depression.
"Suicide," says Chisari, "is one of the complications of interferon treatment."
The Cup Runneth Over
Because of the need for new and better drugs to treat people who are chronically infected with hepatitis C virus, and because of the lack of any vaccine to prevent people from contracting the disease, Chisari and many other scientists worldwide have been trying to find ways to elucidate details of the viral life-cycle and to find new ways to defeat it.
While they have made great strides, their efforts have been hampered by the lack of a good cell culture system in which hepatitis C virus could replicate inside living cells. There are plenty of cell lines derived from human liver tissue. However, all previous attempts to infect these hepatocyte cell lines with hepatitis C virus and get the virus to grow in the cells and produce more virus have failed.
A few years ago, a scientist named Ralf Bartenschlager developed a forerunner of Chisari's replication system, called the replicon system—a line of human liver cells transfected with a portion of the viral genome composed of the non-structural genes only. Inside the replicon cells, the viral RNA is able to replicate. However, because it does not have the ability to make its own structural proteins, it cannot make infectious particles and therefore cannot infect new cells.
The development of this system was a breakthrough at the time, says Chisari, because it allowed scientists to study certain aspects of the viral life-cycle impossible to look at before—particularly replication of the viral genome. It also enabled scientists to propose potential drugs to interrupt viral replication in the replicon system.
However, replication is not the only part of the viral life-cycle that could be disrupted with drugs. Other potential processes to target include viral trafficking in a cell, viral egress (exit) from an infected cell, and viral entry into a new cell. Blocking any one of these could benefit someone who is infected with hepatitis C virus. So far, however, scientists know little about these processes, and there has not been a system in place to move these studies forward.
Until now.
Last year Takaji Wakita of the Tokyo Metropolitan Institute for Neuroscience obtained samples of a strain of hepatitis from a patient whose liver was nearly destroyed by the virus, which had inflicted a particularly nasty bout of "fulminant" hepatitis. But the patient miraculously made a full recovery. Wakita isolated the viral RNA from this patient's blood and created a new replicon with it. Then Wakita tried something that had been tried many times before but never successfully. He transfected the entire RNA into a cell and made an infected cell line that could produce virus that would infect further cells—essentially the elusive cell culture system that scientists had been searching for.
The problem was that Wakita's system wasn't robust. While he had managed to make infectious virus in vitro, his system was inefficient and hard to work with. The rate of infection of new cells from already infected ones was so low that some scientists at a meeting in Heidelberg, Germany last September where Wakita presented his results were said to have viewed it as a glass half empty. For Chisari, however, the glass was not only half full—it was spilling over the edge of the rim. He was not at that meeting because he was spending time with family—his latest granddaughter was born the same day Wakita gave his talk. His laboratory members were there, though, and excited to hear about the development, Chisari wrote to Wakita to obtain a sample of the RNA.
Chisari then took four members of his laboratory—Zhong, Gastaminza, Cheng, and Kapadia—and he put them to work trying to improve the efficiency of Wakita's system. The team transfected the RNA they had received from Wakita into new human liver cells that were more permissive for infection. In an upcoming issue of the journal Proceedings of the National Academy of Sciences, the team describes how it was able to produce a new system in which the hepatitis C virus could replicate inside the cells, making infectious particles that could then go on and infect new cells.
This sort of "cell culture" system offers scientists the possibility of looking at the complete life-cycle of the virus. This discovery also opens the door for high-throughput screening of compounds that block new stages of the viral lifecycle, such as viral entry. This should increase the number of targets for drug and vaccine discovery and make those already out there more accessible.
The article, "Robust hepatitis C virus infection in vitro" by Jin Zhong, Pablo Gastaminza, Guofeng Cheng, Sharookh Kapadia, Takanobu Kato, Dennis R. Burton, Stefan F. Wieland, Susan L. Uprichard, Takaji Wakita, and Francis V. Chisari will appear in the June 28, 2005 issue of the journal Proceedings of the National Academy of Sciences. See: http://dx.doi.org/10.1073/pnas.0503596102
This work was supported by the National Institutes of Health, the Sam and Rose Stein Charitable Trust, the Program for Promotion of Fundamental Studies in Health Sciences of the Pharmaceuticals and Medical Devices Agency and by the Research on Health Sciences focusing on Drug Innovation from the Japan Health Sciences Foundation. Additional support was given through the American Cancer Society–Gloria Rosen Postdoctoral Research Fellowship.
Send comments to: jasonb@scripps.edu
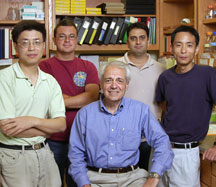 Collaborating on the new system were (left to right): Jin Zhong, Pablo Gastaminza, Francis Chisari, Sharookh Kapadia, and Guofeng Cheng. Photo by Tom Gatz/BioMedical Graphics.
Collaborating on the new system were (left to right): Jin Zhong, Pablo Gastaminza, Francis Chisari, Sharookh Kapadia, and Guofeng Cheng. Photo by Tom Gatz/BioMedical Graphics.
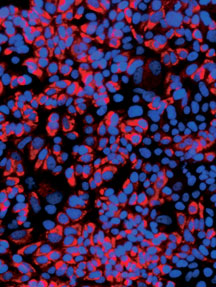
Robust HCV Infection in vitro. Click to enlarge.
